Upon hearing about the symptoms, a health-care provider will formulate a list of possible diagnoses. He or she will ask questions about the symptoms, medical and surgical history, smoking and work history, and other questions about lifestyle, overall health, and medications.
Unless severe hemoptysis is occurring, a chest x-ray will most likely be performed first to look for a cause of the respiratory symptoms.
The x-ray film may or may not show an abnormality.
Types of abnormalities seen in lung cancer include a small nodule or nodules or a large mass.
Not all abnormalities observed on a chest x-ray are cancers. For example, some people develop scarring and calcium deposits in their lungs that may look like tumors on a chest x-ray film.
In most cases, a CT scan or MRI of the chest will further define the problem.
If symptoms are severe, the x-ray may be skipped and a CT scan or MRI may be performed right away.
The advantages of CT scan and MRI are that they show much greater detail than x-rays and are able to show the lungs in three dimensions.
These tests help determine the stage of the cancer by showing the size of the tumor or tumors.
They can also help identify spread of the cancer into nearby lymph nodes or certain other organs.
If a person's chest x-ray film or scan suggests that a tumor is present, he or she will undergo a procedure for diagnosis.
This procedure involves collection of sputum, removal of a small piece of the tumor tissue (biopsy) or a small volume of fluid from the sac around the lung.
The retrieved cells are reviewed under a microscope by a doctor who specializes in diagnosing diseases by looking at cell and tissue types (a pathologist).
Several different ways exist to obtain these cells.
Sputum testing: This is a simple test that is sometimes performed to detect cancer in the lungs.
Sputum is thick mucus that may be produced during a cough.
Cells in the sputum can be examined to see if they are cancerous. This is called cytologic review.
This is not a completely reliable test. If negative, the findings usually need to be confirmed by further testing.
Bronchoscopy: This is an endoscopic test, meaning that a thin, flexible, lighted tube with a tiny camera on the end is used to view organs inside the body.
Bronchoscopy is endoscopy of the lungs. The bronchoscope is inserted through the mouth or nose and down the windpipe. From there, the tube can be inserted into the airways (bronchi) of the lungs.
A tiny camera transmits images back to a video monitor.
The physician operating the bronchoscope can look for tumors and collect samples of any suspected tumors.
Bronchoscopy can usually be used to determine the extent of the tumor.
The procedure is uncomfortable. A local anesthetic is administered to the mouth and throat as well as sedation to make bronchoscopy tolerable.
Bronchoscopy has some risks and requires a specialist proficient in performing the procedure.
Needle biopsy: If a tumor is on the periphery of the lung, it usually cannot be seen with bronchoscopy. Instead, a biopsy is taken through a needle inserted through the chest wall and into the tumor.
Typically, a chest x-ray or CT scanning is used to guide the needle.
This procedure is safe and effective in obtaining sufficient tissue for diagnosis. After the chest surface is cleaned and prepared, the skin and the chest wall are numbed.
The most serious risk with this procedure is that the needle puncture may cause an air leak from the lung (pneumothorax). This air leak occurs in as many as 3%-5% of cases. Although this condition can be dangerous, it is almost always recognized and treated without serious consequences.
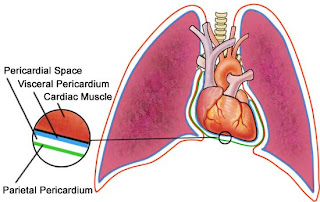
Thoracentesis: Lung cancers, both primary and metastatic, can cause fluid to collect in the sac surrounding the lung. This fluid is called a pleural effusion.
The fluid usually contains cells from the cancer.
Sampling this fluid can confirm the presence of cancer in the lungs.
The fluid sample is removed by a needle in a procedure similar to needle biopsy.
Thoracentesis can be important for both staging and diagnosis of the condition.
Thoracotomy: Sometimes a lung cancer tumor cannot be reached by bronchoscopy or needle procedures.
In these cases, the only way to obtain a biopsy is by performing an operation.
The chest is opened (thoracotomy), and as much of the tumor as possible is removed surgically. The removed tumor is then examined microscopically.
Unfortunately, this operation may not be successful in removing all tumor cells if the tumor is large or has spread to the lymph nodes outside of the lungs.
Thoracotomy is a major operation that is performed in a hospital.
Mediastinoscopy: This is another endoscopic procedure. It is performed to determine the extent that the cancer has spread into the area of the chest between the lungs (the mediastinum).
A small incision is made into the lower part of the neck, above the breastbone (sternum). A variation is to make the incision in the chest.
A mediastinoscope is inserted behind the breastbone.
Samples of the lymph nodes are taken to evaluate for cancer cells.
Mediastinoscopy is a very important step to determine whether the tumor can be surgically removed or not.
Other tests: Other tests are performed to stage the tumor and to assess a person's ability to withstand surgery and other treatment.
Pulmonary function tests assess breathing capacity.
Blood tests are performed to identify any chemical imbalances, blood disorders, or other problems that might complicate treatment.
CT scans or MRIs may be performed on the most common areas of spread to check for metastatic disease. These tests are generally performed only if symptoms occur that suggest metastatic disease. Certain treatment protocols require that these tests be performed.
A bone scan can determine whether the cancer has spread to the bones.
Staging: Staging is a method of classifying the tumor for purposes of treatment planning.
Staging is based on size of the tumor, location of the tumor, and degree of metastasis of the tumor (if any).
The treatment will be individually tailored to the tumor stage.
Tumor stage is related to the outlook for cure and survival (prognosis). The higher the tumor stage, the less likely the disease will be cured.